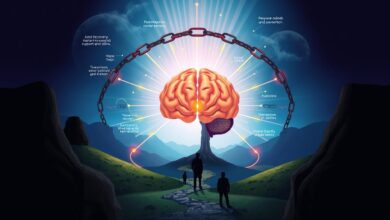
disease model of relapse prevention

Addiction is a complex condition that affects people at a neurological level. It needs ongoing management and treatment. The disease model sees addiction as a chronic, relapsing brain disease. It involves compulsive drug seeking and use, despite harmful effects.
This model shows that addiction is not a personal choice or moral failing. It is influenced by genetic, biological, and environmental factors.
Understanding addiction through the disease model helps in facing relapse prevention and long-term recovery challenges. It compares addiction to chronic diseases like diabetes or heart disease. This shows the need for a comprehensive, evidence-based treatment approach.
Adopting the disease model can also reduce stigma and shame around addiction. It encourages more compassion and empathy towards those struggling with it.
Seeing addiction as a chronic, relapsing brain disease is key to effective relapse prevention and long-term recovery. This model stresses the importance of ongoing care and tailored treatment. It also highlights the need for protective mechanisms to manage the condition and prevent future relapses.
Table of Contents
Understanding the Disease Model of Addiction
The disease model of addiction sees addiction as a chronic, relapsing brain disease. It has key features that set it apart from other problems or choices. This model is widely accepted.
Primary Characteristics of the Disease Model
Addiction is seen as a primary disease, not just a symptom. It’s a chronic disorder with compulsive behavior despite negative effects. The model says addiction has genetic, psychosocial, and environmental factors like other chronic diseases.
Role of Brain Function in Addiction
Addiction changes brain function, especially in reward, motivation, and decision-making areas. Research shows substance use can release dopamine up to 10 times more than usual, affecting the brain’s reward system. This can lead to tolerance and dependence.
Chronic Nature of Addiction
The disease model sees addiction as chronic, needing long-term treatment and support. Recovery allows the brain to heal, with new connections forming to overcome addiction. But, the risk of relapse is always there, and ongoing management is key to staying sober.
| Key Aspects of the Disease Model | Implications for Understanding and Treating Addiction |
|---|---|
| Addiction is a primary, chronic, and relapsing brain disease | Addiction requires long-term, comprehensive treatment and support, similar to other chronic conditions |
| Addiction has genetic, psychosocial, and environmental risk factors | Personalized treatment approaches that address multiple factors are essential for success |
| Addiction involves significant alterations in brain function and structure | Targeted interventions that address the neurobiological aspects of addiction can be effective |
“Addiction affects the prefrontal cortex, impairing judgment and self-control, making it harder to resist cravings and increasing the risk of relapse.”
Neurobiology of Addiction and Recovery
Addiction is a complex brain disease that changes the brain’s structure and function. The mesolimbic dopamine system, key in the brain’s reward pathway, is crucial in addiction. Substance use can make this system less sensitive to natural rewards, leading to a strong desire for drugs or addictive behaviors.
The brain’s reward pathway is hijacked in addiction. This leads to intense cravings and withdrawal symptoms. It also affects decision-making and the brain’s stress response system. These changes can last long after stopping substance use, making addiction chronic and relapse risky.
Studies using functional neuroimaging have shed light on addiction’s neural circuits. They’ve found brain regions and networks linked to reward, control, stress, emotions, and learning. These areas are affected in those with substance use disorders.
| Key Neurobiological Changes in Addiction | Impact on Behavior and Recovery |
|---|---|
| Dysregulation of the dopamine system in the mesolimbic reward pathway | Reduced sensitivity to natural rewards, increased drive for drugs or addictive behaviors |
| Impaired prefrontal cortex function | Difficulty in decision-making, impulse control, and regulation of emotions |
| Disruption of the brain’s stress response system | Increased vulnerability to stress and heightened cravings during periods of abstinence |
Understanding addiction’s neurobiological mechanisms is key to effective treatment. By addressing brain changes, healthcare professionals can help individuals regain control. This supports long-term recovery and a fulfilling life.
“Addiction is a brain disease expressed in the form of compulsive behavior. It is not simply a weakness of willpower or a moral failing.”
Disease Model of Relapse Prevention
The disease model sees addiction as a long-term condition that needs constant care. It highlights the need to know your relapse triggers, find good coping strategies, and make a safety plan for lasting recovery.
Key Components of Prevention
Understanding what might lead to relapse is key in this model. It’s about spotting your high-risk situations and emotional states that might pull you back to drugs. By learning to handle these tough times, you can stay on the path to recovery.
Identifying Risk Factors
This model asks you to look at your life and habits to find relapse triggers. These could be places, people, feelings, or even certain smells that make you want to use. Knowing these can help you plan how to avoid or deal with them.
Building Protective Mechanisms
For lasting recovery, the model stresses the need to build strong defenses. This means having a good support network, trying proven therapies, and making healthy lifestyle choices. By doing this, you can grow stronger and lower your chance of relapsing.

The disease model shows that addiction is a serious and complex issue. By focusing on prevention, identifying risks, and building defenses, you can face the recovery journey with more strength. This can help you stay sober for a long time.
Genetic and Environmental Influences
Addiction is a complex disease, shaped by both genetics and environment. Researchers are working hard to find the specific genes linked to addiction risk.
Studies show that genetics play a big role, about 50% of the risk. Some people are more prone to addiction because of their genes. Family history also matters a lot, showing addiction can run in families.
But, environment also plays a big part. Things like trauma, bad social environments, and easy access to drugs can lead to addiction. Childhood trauma, for example, can increase the risk of addiction later on.
| Substance Use Disorder | Sample Size of Largest GWAS | SNP-heritability | Independent Variants/Genes Identified | Genetic Correlation Between Use and Use Disorder |
|---|---|---|---|---|
| Alcohol Use Disorder | 435,563 | 0.07 | 29 / 66 | 0.77 |
| Drinks per Week | 941,280 | 0.04 | 99 / 362 | 0.47 |
| Nicotine Dependence | 58,000 | 0.09 | 5 / 16 | 0.4 – 0.5 |
| Ever Smoked | 1,232,091 | 0.08 | 378 / 833 | 0.47 |
| Cannabis Use Disorder | 384,925 | 0.12 | 2 / 3 | 0.50 |
| Ever Used Cannabis | 184,765 | 0.11 | 8 / 35 | 0.51 |
| Opioid Use Disorder | 639,709 | 0.13 | 10 / 4 | N/A |
| Cocaine Use Disorder | 6,546 | 0.30 | 1 / 5 | N/A |
The mix of genetics and environment makes addiction a complex disease. Knowing this is key to creating effective prevention and treatment plans. These plans should tackle both personal risks and outside factors.
“Addiction is a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite negative consequences.”
Treatment Approaches in Recovery
Overcoming substance use disorders requires a detailed and proven plan. The disease model of addiction shows these conditions are chronic. This means they need ongoing care and support.
Evidence-Based Interventions
Good treatment mixes medication-assisted treatment and behavioral therapies. Medications target brain receptors to reduce cravings and manage withdrawal. Behavioral therapies, like cognitive-behavioral therapy, help change negative thoughts and behaviors linked to substance use.
Medication-Assisted Treatment
Medications like buprenorphine, methadone, and naltrexone are very effective for opioid use disorders. They block opioid effects, cut cravings, and stop relapse. With counseling and support, these treatments greatly improve recovery chances.
Behavioral Therapies
Behavioral therapies, such as cognitive-behavioral therapy (CBT), teach coping strategies and managing triggers. CBT helps individuals face and change negative thoughts that lead to substance use. Support groups, like Alcoholics Anonymous, offer a network of support and shared experiences in recovery.
Using a detailed, evidence-based approach that covers physical, mental, and social aspects of addiction boosts recovery chances. This way, individuals can achieve long-term sobriety and better overall well-being.
Role of Support Systems
Recovering from addiction is a tough journey that needs a lot of support. Peer support groups, family help, and community resources are key. They help people deal with addiction as a long-term condition.
Peer support groups offer a sense of belonging and hope. They let people share their stories of addiction and recovery. Studies show that those who joined groups like Alcoholics Anonymous (AA) were less likely to slip back into addiction.
Family support is also very important for recovery. Being around positive people can help prevent relapse. Research finds that more social support means lower substance use after treatment.
Also, community resources like counseling, job training, and housing help tackle addiction’s effects on life. These services support self-care, seeking help, and changing bad habits. All these steps help avoid relapse.
The disease model of addiction highlights the need for strong support systems. With peer support, family help, and community resources, people can build a solid recovery base.
“Addiction recovery is a journey, not a destination, and the support of others can make all the difference.”

In summary, support systems are crucial for overcoming addiction. Using these resources boosts the chances of staying sober for a long time.
Managing Triggers and High-Risk Situations
Recovery is tough, with many triggers and risky situations that can lead to relapse. It’s key to know these dangers and find ways to deal with them. This helps keep you sober for a long time.
Identifying Personal Triggers
Start by figuring out what triggers you. These can be feelings, places, social events, or even smells that make you want to use. Common ones include stress, feeling down, being around people who use, and big changes in life.
Developing Coping Strategies
After knowing your triggers, it’s time to find ways to handle them. Try stress management techniques like meditation, deep breathing, or exercise. Mindfulness techniques help you stay focused and avoid bad thoughts that might lead to relapse.
Creating Safety Plans
Having a safety plan is also important. This plan should list people you can call, safe places to go, and how to leave a bad situation. Being ready helps you get through tough times and avoid relapse warning signs.
Handling triggers and risky situations is a constant effort. Stay alert and keep working on your recovery. With a good plan and the right strategies, you can stay strong and achieve lasting sobriety.
Lifestyle Modifications for Long-term Recovery
Recovering from addiction is more than just treatment. It’s about building healthy habits, managing stress, and focusing on self-care. These steps are key to staying sober and avoiding relapse.
Exercise and a healthy diet help your body and mind heal. Stress-reducing activities like meditation or yoga are also helpful. Trying new hobbies and interests can distract you from old habits. Regular medical check-ups and mental health care are also important for managing addiction.
| Lifestyle Modification | Benefits for Long-term Recovery |
|---|---|
| Regular Exercise | Improves physical and mental health, boosts mood, and reduces cravings |
| Balanced Nutrition | Supports the body’s recovery, replenishes nutrients, and stabilizes energy levels |
| Stress Reduction Practices | Helps manage chronic stress, improve emotional regulation, and prevent relapse |
| Developing New Hobbies | Provides positive alternatives to substance use, enhances mood, and increases self-esteem |
| Ongoing Medical and Mental Health Care | Ensures comprehensive management of addiction as a chronic condition |
By making these lifestyle changes, people in recovery can better prevent relapse. They also improve their overall health and well-being.
“Addiction is a chronic disease, and recovery is a lifelong process. Adopting healthy lifestyle choices is essential for maintaining long-term sobriety and preventing relapse.”
Conclusion
The disease model of relapse prevention shows that addiction is a long-term issue. It highlights the need for constant care and support in your recovery journey. By understanding addiction’s roots and your personal triggers, you can find ways to stay sober and healthy.
Good treatments mix medicines, behavioral therapies, and a strong support network. This mix gives you the tools to face addiction’s challenges. Remember, recovery is a journey that never ends. It needs your ongoing effort and the help of healthcare teams, family, and friends.
Starting your recovery journey means seeing addiction as a chronic disease. With the right strategies and ongoing care, you can overcome it. Focus on managing your disease and getting constant support to achieve lasting success and well-being.
FAQ
What is the disease model of addiction?
The disease model sees addiction as a chronic brain disease. It’s marked by a strong urge to use drugs despite harm. It’s not a choice or a moral failing, but a condition affecting the brain.
What are the key features of the disease model of addiction?
Key features include addiction being a chronic and progressive brain disease. It’s driven by a strong urge for rewarding stimuli, even when it’s harmful. It’s seen as a primary disease, not just a symptom, with genetic, psychosocial, and environmental factors at play.
How does the disease model explain the neurobiological mechanisms of addiction?
Addiction changes the brain’s reward system. Repeated drug use can mess up the dopamine system. This leads to a reduced response to natural rewards and a strong drive for drugs or addictive behaviors.
What are the key components of the disease model of relapse prevention?
The model sees addiction as a chronic condition needing ongoing management. It focuses on understanding personal triggers, developing coping strategies, and creating safety plans to prevent relapse.
How do genetic and environmental factors contribute to addiction?
Genetics play a big role, with about half of a person’s risk coming from their genes. Environmental and social factors also matter, like unaddressed trauma, family history, early drug exposure, and high-risk environments.
What are the evidence-based treatment approaches aligned with the disease model?
Treatments focus on giving people tools to manage their addiction. This includes medication-assisted treatment and behavioral therapies like cognitive-behavioral therapy.
How do support systems help in addiction recovery?
Support systems are vital for recovery. Peer support groups, family involvement, and community resources help address addiction’s impact on life. They provide the support needed to manage addiction as a chronic condition.
How can individuals manage triggers and high-risk situations to prevent relapse?
Managing triggers and high-risk situations is key to preventing relapse. It involves identifying personal triggers, developing coping strategies, and creating safety plans for difficult situations.
What role do lifestyle modifications play in maintaining long-term recovery?
Lifestyle changes are crucial for long-term recovery. Adopting healthy habits like regular exercise, balanced nutrition, and enough sleep is important. So is finding new hobbies and using stress reduction techniques.